The current pandemic represents a colossal medical conundrum involving all aspects of healthcare. We realized early on that the entire global scientific community was attempting to optimize the results of several overlapping, competing, and parallel realities that were all emerging and evolving with differing time signatures. After we had orchestrated all of the evolving data, it became glaringly obvious that a complete paradigm shift was the only way to solve this conundrum. The insight required a refocusing of the problem by turning the efforts backward and recognizing the problem is emerging. Moving forward, the answer to the conundrum lies in treating the patient as the source of the problem and focusing all of our attention to that source.
This current paper tackles the current problem head on by focusing our attention on stopping the virus in the patient’s respiratory tract, at its source. Heretofore, we never tried to stop the virus from getting out and onto our personal protective equipment from the very beginning. Logically, the only thing that makes sense is to contain the COVID virus in the human respiratory tract, right at its source, rather than trying to deactivate it or trap it once it comes out of the body and contaminates our working environment and puts our health care workers at risk. The purpose of the paradigm shift as the ultimate answer to this conundrum also answers the main question lurking in the consciousness of all health care workers; are we safe now and have we ever really been safe up to this point. How could such a simple solution have defied logic for so long?
HEPA (high efficiency particulate air) filtration is a common denominator in Ambu bags used in operating rooms across the nation. Attached to the orifice of the simple face mask, the bidirectional HEPA filter has the ability to capture airborne viral and bacterial micron particles with an efficiency of at least 99.99% (EPA, 2020) compared to the standard N95 mask’s 95% efficiency rate. This Ambu mask and HEPA filter have been used across the nation during routine intubations, offering increased protection to healthcare workers exposed to aerosolized secretions of the human airway as well as protecting the anesthesia machine.
become the main path of transmission to healthcare workers on the frontline and with the impossibility to accurately distinguish between asymptomatic carriers and healthy individuals, it only makes sense to treat the airway of all individuals as a possible vehicle for the transmission of infection. Heretofore, Infectious Disease committees were constantly striving for ways to protect the patient from a nosocomial infection. Once again, the paradigm shift requires us all to think that the patient is the source of the infection. In an effort to contain the nation’s consistently dwindling supply of PPE, on which the US alone has spent over ten billion dollars (Toner, 2020), it is imperative to focus attention on alternative ways of containing the virus at its source before it has the chance to initiate pathogenesis in our health care workers. While the entire scientific community continues to work on a solution, good people are dying. The proposed paradigm shift of fitting patients with a bidirectional HEPA-filtered face mask before elective outpatient procedures not only promotes the life and wellbeing of healthcare workers while protecting the patient, but also allows for the revival of an otherwise shattered healthcare industry. Our proposed hypothesis is a solution to allow a safe best practices model to bring our outpatient surgery healthcare system back online.
The Focus It became apparent early on that accurately testing for coronavirus on a large scale with a quicker turnaround time for results was an obstacle not so easily overcome. Early testing measures took days for patients to receive their results, rapid testing now only takes fifteen minutes, but the results are not always accurate. A study done by the Cleveland Clinic found that the rapid testing only detected the virus in 85.5% of the tested samples. To put that into perspective, if one were to test 100 positive patients, the rapid testing kits would result in a false negative in at least fifteen patients (Stein 2020 citing Procop 2020). New tests and treatments continue to gain emergency FDA approval every week with very little vetting. The accuracy of such emergently approved testing kits and treatments lends a certain ambiguity of never truly knowing the true movements of SARS-CoV-2 in our workplace environment. This fatal flaw inevitably leads to potential increased viral loads with each exposure of the virus to the healthcare providers who believe the patient has tested negative; this shadow of doubt is simply unacceptable. As the response to the virus evolves, each new solution becomes the next problem. We know the potential is there for the virus to mutate. We also learned from the Spanish flu that waves of this new virus can and will occur (Dr. Fauchi).
The only way to protect the lives of frontline health care workers is to seal off the source of the infection as safely and efficiency as possible. Likewise, the nature of the beast that is SARS-CoV-2 is one that we have never seen before and the trajectory of its transmission is as mysterious as the virus’s true origins. Søren Kierkegaard stated that “life can only be understood backwards…but must be lived forwards.” (Journals IV.A.164 1843). The CDC reminds us that the 1918 influenza pandemic occurred in three waves, and was the most severe pandemic in history. The first wave was in the spring of 1918, the second wave was in the fall of 1918 and the third wave was in the winter of 1918. Initially, there was no recommendation for people wear masks. Now the CDC guidelines recommends wearing a mask and self distancing (2020). However, a study conducted in China found virus particles within the ventilation systems of hospitals caring for COVID-19 patients, leading experts to determine that forward momentum of the turbulent gas cloud of respiratory emissions can actually be up to twenty-seven feet (Bourouiba, 2020). As the situation continues to change daily and the possibility of vaccines forthcoming, the threat of a “second and third wave” is potentially on our horizon; the only way to protect the lives of frontline healthcare workers is to seal off the source of infection as safely and efficiently as possible.
COVID-19 has collectively become a rude awakening. Up to this point in time, our infection control measures have all centered on keeping the patient free from an infectious disease when they enter our institutions. Nowhere else in history have we come to the realization that we must now protect ourselves from the patient on such a large scale. Moving forward, every possible measure should be taken to decrease the likelihood of potential exposures of healthcare workers to infectious pathogens, we cannot continue to rely on testing and good faith that the patient will quarantine themselves prior to their procedure. In the real world, this simply is not possible. We must now make this paradigm shift and take deliberate action to change the universal precautions that have catastrophically failed in such a critical moment in human history; it has become all too apparent that current practice and preparedness measures for the protection of healthcare workers is woefully inadequate. As there is currently no known vaccine for SARS-CoV-2, one must assume it will remain a threat to human life ongoing; patients entering hospitals should be mandated to wear bidirectional HEPA-filtered face masks as a rule going forward to protect our health care workers.
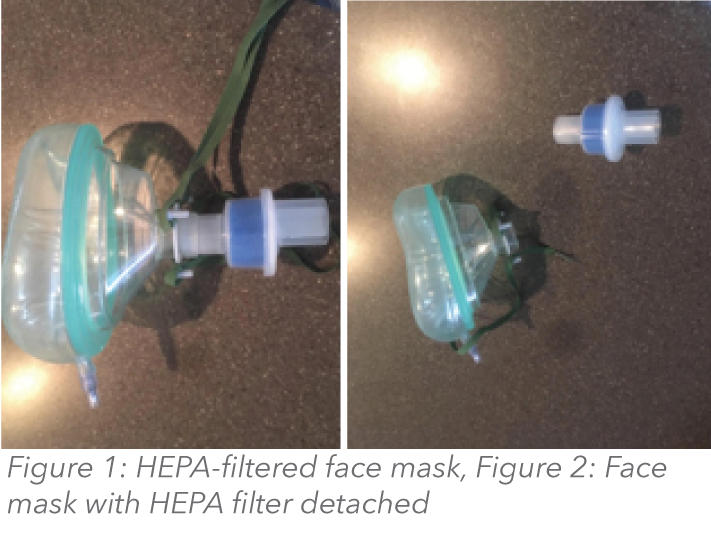
Figure 2 outlines a proposed process where in an ideal situation, the patient will have never exhaled their potentially contaminated respiratory tract into our health care environment without having the airway column filtered and contained.
The Implementation Several days prior to any elective procedure, patients should be directed to the Durable Medical Equipment (DME) Department or Occupational Health to be fitted with a bidirectional HEPA-filtered mask. They should show up to the Durable Medical Equipment Department or Occupational Health office wearing a simple cloth or surgical mask, if they do not have access to a mask, they should be provided one before being allowed entry to the building. Universal temperature and pulse oximetry monitoring must be implemented early on in the DME Department. Men with facial hair will be required to shave in order to be properly fitted for their masks. After being fitted for the bidirectional HEPA-filtered mask, they should be instructed with the teach-back method on the proper technique of donning and doffing of the mask, storage, and hand hygiene as well as given written instructions for further education.
Patients will be registered for their outpatient procedure via Teleregistration and a preoperative Telemedicine visit with the Anesthesia Department will be required for patients who are to receive certain medications by mouth prior to procedure. In order to limit the amount of contaminated air expelled by the patient while in the hospital setting, they will be instructed on taking these medications, as well as inhalers, at home the day of the procedure and informed of the new standard use of anti-secretory agents, such as glycopyrrolate, by Pre-Anesthesia. Prescriptions for these medications may need to be provided preoperatively. Alternative routes of administration of medication may be taken into consideration on a patient-by-patient basis. It is up to the discretion of the anesthesia department to make those determinations during the preoperative screening process.
On the day before the procedure, Same Day Surgery will contact the patient and reconcile medications as well as provide standard instructions. The patient will be told to wear a button down shirt or zippered hoodie in order to properly doff their personal clothing to avoid pulling a shirt up over the mask in an effort not to compromise the seal of the bidirectional HEPA filter mask. They will also be informed to bring their health insurance cards and identification in a zip-locked bag. On the day of procedure, patients will apply their mask in their car prior to entry into the building where a CNA/CMA transporter will pick them up by way of wheelchair and document their temperature and pulse oximetry. If their pulse oximetry is low, COVID would be suspected and the patient will be referred to the Emergency Department for further testing. They will show their zip-locked bag of health insurance and identification at registration prior to being escorted to Same Day Surgery. Any necessary lab draws can be performed at the bedside in the preoperative holding area by qualified staff members. Extra care and precaution should be taken for patients with maxillofacial irregularities that do not allow for proper seal of bidirectional HEPA-filtered masks as well as pediatric patients who have a tendency to fidget with face masks. Alternative measures should thus be explored as a proper seal of the mask must be maintained to allow for maximum pathogen containment and the safety of healthcare workers; use of bidirectional HEPA-filtered masks may be contraindicated in these individuals and alternative measures should thus be explored.
In a perfect scenario, the only two instances where the bidirectional HEPA-filtered mask is intentionally removed in the hospital setting is just prior to intubation and immediately following extubation. In order to prevent subsequent exposure to aerosolized pathogens, intubation and extubation should be performed underneath a hood or acrylic box barrier. Two large Yankauer suctions will be held at the corner of the patient’s mouth on either side, producing a negative pressure effect that draws and traps the infected air column into the Neptune suction system. Once the patient is intubated, the contaminated column of air is now captured into the Scavenger system of the anesthesia machine. Once the surgery is completed, the Anesthesiologist will reverse and repeat the sequences. During the extubation phase, the Anesthesiologist will deeply extubate the patients utilizing Lidocaine in the airway to decrease bucking on the tube.
They will then immediately pull the patient’s endotracheal tube out and place their Ambu mask with the bidirectional HEPA filter on immediately after the extubation. Environmental Service workers will clean and sterilize the acrylic box with alcohol immediately. During the extubation, only the anesthesia provider and one other assistant should be in the room during the extubation which has the potential to be the most contaminating portion of the whole process. PPE must still be worn by the healthcare workers providing care, but this process allows hospitals to extend the life of otherwise single-use medical-grade PPE and/or decreases the likelihood of contracting the virus through donning and doffing. Bidirectional HEPA-filtered masks as a perioperative standard of care offer a modern solution to a modern problem and prioritizes the wellbeing of the healthcare workers sacrificing on the front lines of the coronavirus pandemic.
References
Bourouiba, L. (2020). Turbulent Gas Clouds and Respiratory Pathogen Emissions. Jama. doi: 10.1001/jama.2020.4756 Ofgang, E. (2020, April 10). CT companies building intubation boxes for hospitals. Retrieved from https://www.connecticutmag.com/the-connecticut-story/ct-companies-building-intubation-boxes-for-hospitals/article_751d5ffc-7b5e-11ea-a599-63f9313dc11b.html
Running Essential Errands. (2020, April 10). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/essential-goods-services.html Stein, R. (2020, April 21). Study Raises Questions About False Negatives From Quick COVID- 19 Test. Retrieved from https://www.npr.org/sections/health-shots/2020/04/21/838794281/study-raises-questions-about-false-negatives-from-quick-covid-19-test Toner, M. (2020). Interim Estimate of the US PPE Needs for COVID-19. Johns Hopkins Center https://www.centerforhealthsecurity.org/resources/COVID-19/PPE/PPE-estimate.pdf What is a HEPA filter? (2019, April 3). Retrieved from https://www.epa.gov/indoor-air-quality- iaq/what-hepa-filter-1
Article by: Dale R. Chilson, D.O., FAOCO & Tracey Delgado BSN, RN Otolaryngology & Facial Plastic Surgery St. Margaret's Hospital, Spring Valley, Illinois